Dry eye syndrome, also known as dry eye disease, is the most common reason for a visit to an eye doctor. Dry eye syndrome is a common condition almost everyone has been through. However, many people complain about how hard it is to find a clear solution to this syndrome. Dry eye disease is a multifactorial disease, and patients have various symptoms and signs, such as ocular pain, visual dizziness, and rapid decrease and evaporation of tears.
When we blink, newly formed tears cover the surface of our eyes. The amount of tear secreted could be decreased, or the tear can evaporate rapidly. This happens when tear evaporation is promoted in a dry environment. Even if tears are reduced due to aging or inflammatory diseases such as Sjogren syndrome, an autoimmune disease. Dry eye syndrome occurs when there is a problem with the “tear film.” If the tear film becomes unstable, dry eye symptoms occur.
Symptoms and Signs
These dry eye symptoms can range from minor to severe symptoms. Typical symptoms of dry eye syndrome are unpleasant feelings and abnormal eye dryness. People with dry eyes may feel sore and pressed. Also, wind and intensive light can cause eye irritation. Chronic inflammation with worse eye symptoms might be progressed by a specific disease, which interferes with mucin secretion and inhibits mucus layer formation. Dry eyes have been classified into two categories: aqueous deficiency and evaporative dryness. However, the two are not mutually exclusive, and many patients have a combination of these two causes.
- Dry feeling in the eyes
- When the wind blows, more tears pour out.
- Stinging, burning, or a feeling of pressure in the eyes.
- A sandy, gritty, or foreign body sensation.
- Epiphora, or tearing, is a symptom that is often counterintuitive. This is due to dryness leading to pain or irritation that results in intermittent excess tearing or epiphora.
- Pain is a broad term, and sharp and dull pain can be described as localized to some part of the eye, behind the eye, or even around the orbit.
- Redness is a common complaint and is often made worse by the rebound effect of vasoconstrictors found in many over-the-counter eye drops designed to reduce redness. Vasoconstrictors may decrease redness for the short term by constricting the vessels of the episclera but can have a rebound effect and increased redness after the drops wear off in a relatively short time period.
- Blurry vision, particularly intermittent blurry vision, is a common complaint and may also be described as glare or haloes around lights at night.
- Vision fluctuation and difficulties in reading.
- A sensation of heavy eyelids or difficulty opening the eyes.
- Excessive blinking.
- Eyelid twitching.
- Dryness is a common problem for contact lens wearers, and irritation may make contact lenses uncomfortable or even impossible to wear.
- Tired eyes. Closing the eyes may provide relief to some individuals with dry eyes.
- Inability to cry in severe DED.
- a feeling of foreign matter that looks like grains of sand in one’s eyes
What is Tear Film?
Tear film on the eyes is a barrier that keeps the eyes soft and wet and prevents eye diseases. The tear film is approximately 2 to 5 µm thick over the cornea. The tear film maintains the eyes in a balance of nutrition and oxygen for its healthy ocular structures.
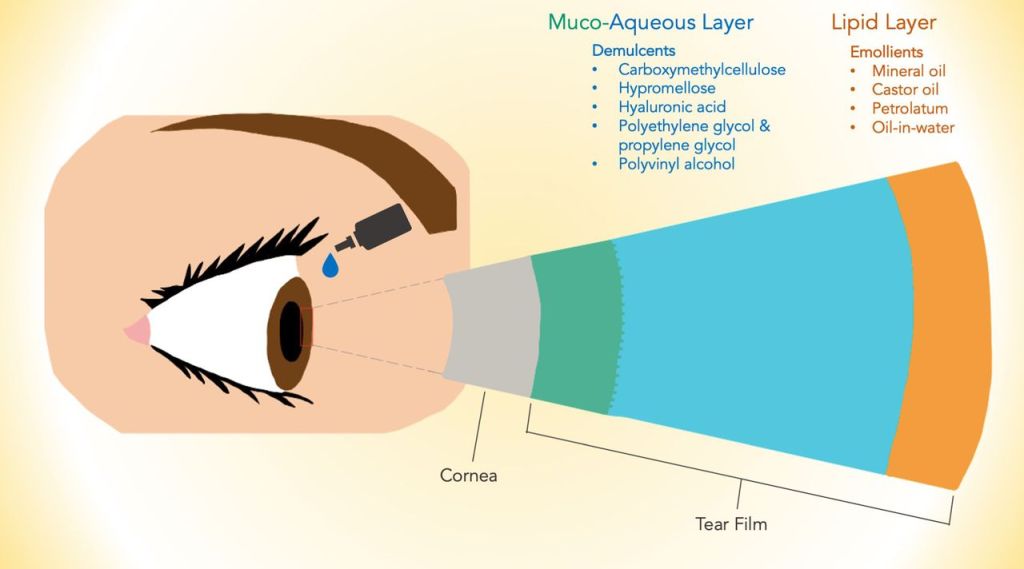
The tear film consists of three layers from inside to outside: mucus layer, aqueous layer, and lipid layer. Each layer has its own role. The innermost layer is called the mucin layer. This basal layer comprises mucins, or glycoproteins. Mucin is secreted by the goblet cell of the conjunctiva and allows tears to stick to the eyes. Suppose this mucus layer is not working correctly. In that case, the tears are not stably attached to the eyes anymore. Even if artificial tears are used due to lack of mucin, tears fall off from the cornea.
The middle layer is the aqueous layer. It occupies most of the tear film, and it is the thickest component of the tear film. This layer is crucial in ocular health, and water is secreted by the tear gland. This water layer nourishes the eyes and protects them with antibacterial substances such as lysosomes, which are vital in preventing eye diseases.
And the last one is the lipid layer, the most superficial barrier. The lipid is secreted from the Meibomian gland of the eyelid. It covers the aqueous layer to reduce the evaporating tears.
Causes of Eye Dry Syndrome
A thin tear film causes inflammation and damage to the eyeball surface. In proportion to the amount and severity, tears in the tear film evaporate.
There are many reasons for these changes in the tear film, including inflammatory conditions, dry environments, hormone changes, and contact lenses.
Overall, dry eye syndrome may occur more often in women, especially menopausal women with hormonal imbalances who are at high risk. Increasing age also plays a significant role in the frequency of disease. Also, eye surgery or long-term medication can cause dry eyes. Many drugs may be associated with dry eyes, such as diuretics, antihistamines, antidepressants, psychotherapy, cholesterol-lowering drugs, beta-blockers, and oral contraceptives.
There may also be other factors in unhealthy tear film, including underlying systemic disease conditions, anatomical abnormalities, and neuropathological dysfunction. Systemic diseases such as diabetes, thyroid disease, rheumatoid arthritis, and Sjogren syndrome need to be accompanied by proper treatments.
In addition to certain conditions, factors such as vision correction, dry air, reduced blinking due to smartphone or computer work, stress, aging, and malnutrition are blamed. Young people can also develop dry eyes due to long-term use of electronic devices such as cell phones and computers.
Dry eyes are caused by an imbalance in the tear film, causing excessive evaporation of tears. Suppose the tear film becomes unstable due to various reasons. In that case, the film’s thickness is decreased, and you may feel unpleasant symptoms. In proportion to the amount and severity of tear film, most of the tears in the eyeball evaporate, or the water deficiency of the eyeball progresses. Multifacts and lifestyles we discussed may lead us to dry eye syndrome.
Potential Causes and/or Factors Associated with DED
- Systemic drugs: antihistamines, antihypertensive drugs, anti-anxiety drugs/benzodiazepines, diuretics, systemic hormones, nonsteroidal anti-inflammatory drugs, systemic or inhaled corticosteroids, anticholinergics, isotretinoins, antidepressants
- Glaucoma drugs applied to the eyes or preservatives in eye drops
- eczema or skin disease around the eyelids or eyelids
- Meibomian gland dysfunction
- ophthalmic surgery (such as cataract surgery)
- Chemical or thermal damage that injures the conjunctiva
- Allergy
- Looking at the screen without blinking
- Problems with vitamin dosage. Vitamin A deficiency in particular can lead to severe eye damage
- Corneal damage due to wear and tear due to long-term lens use, etc
- graft versus host disease
- Systemic disorders including Sjogren syndrome and other autoimmune or connective tissue disorders and thyroid diseases such as rheumatoid arthritis and lupus
- Environmental factors include exposure to irritants such as chemical fumes, cigarette smoke, pollution, or low humidity
References
- BMJ Open Ophth 2021, 6
- Dry Eye Syndrome / Mark I. Golden; Jay J. Meyer; Bhupendra C. Patel. / National Library of Medicine
- J Ophthalmic Vis Res. 2011 Jul; 6(3): 192–198.
- J Korean Med Assoc 2018;61(6):352-364.
- 약국에서 만난 건강기능식품/노윤정 지음/ 생각비행

댓글 남기기